GENDER AFFRMING SURGERY & RECONSTRUCTIVE UROLOGY
Penile Prosthesis in Transmen
Placement of a penile prosthesis is often the final surgery after a long journey for many transmen – it is the culmination and hopefully last genital surgery. It is also a surgery with a high risk of complications and can potentially compromise the outcome of prior surgeries to create the neo-phallus.
Penile Prosthesis after Metoidioplasty
There are 2 type of masculinizing genital surgeries: the metoidioplasty and some form of a phalloplasty. There is no FDA approved penile implant for a metoidioplasty. There is, however, a new device made by ZSI, which is available in Europe and designed specifically for a metoidioplasty. Essentially the device is made up of 2 silicone rods, each about 4mm in width, with a silver cable in the middle for stiffness. The solid cable is cut intra-operatively based on the length of the neo-phallus. There is not very much data available on this prosthesis and only time will tell if it will work. However, it is currently not available in the United States.
Penile Prosthesis after Phalloplasty
There are 2 kinds of penile prosthesis for phalloplasties: malleable prosthesis and an inflatable prosthesis. The malleable prosthesis is a semi-rigid prosthesis that is always partially erect. Men can bend it down when not having sex and bend it upwards when they want to have sex. It is easy to place surgically and has less component parts so it is less likely to get infected. The problem is that it is never fully soft and never completely hard. Also, in my opinion, different from cis-men it has a higher risk of infection that inflatable prosthesis.
Type of Prosthesis available after Phalloplasty
The inflatable prosthesis allows deflation of the prosthesis and inflation when patients want a rigid phallus. As such, it is more “natural” and patients can have a flaccid phallus when they are not stimulated. The prosthesis come in two varieties – one made up of two components (2 piece inflatable prosthesis) and one made up of three components (3 piece inflatable prosthesis). In the United States, there are two companies that make an FDA approved prosthesis: Coloplast and AMS. There are some differences in the types of prosthesis that both of these companies make including impregnation of the prosthesis with antibiotics to reduce the risk of infection, the ease of use of the pump and varying levels of girth expansion.
Differences in Penile Placement between Transmen and Cismen
Placement of a penile prosthesis in transmen is different then placement in cis-men for a few reasons. First, cis-men’s penis’s contain 2 internal cylinders called the corpora cavernosa. These are the bodies that would normally create erections as they fill up with blood. These cylinders are made up of a tough tissue called the tunica which contains the implants. The corpora prevent migration or erosion of the cylinders into the skin and fix the cylinders in placed so that during sex they don’t move around. When placing a prosthesis in transmen we try to recreate this function by suturing the prosthesis down to the pubic bone to keep it in place and prevent migration. But it is not perfect.
The 3-piece inflatable Prosthesis after Phalloplasty
The 3-piece inflatable prosthesis is the most common type of prosthesis used. It is made up of two inflatable cylinders placed in the penis, a pump placed in the scrotum and a reservoir that contains fluid. When the pump is pressed fluid is transferred from the reservoir to the cylinders. When deactivated, the fluid is transferred back to the reservoir causing the prosthesis to deflate and the erection to go away.
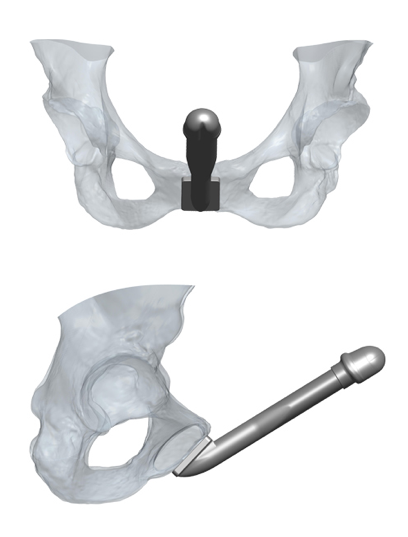
A Penile Implant Specifically for Transmen
There has been an implant designed specifically for phalloplasty: the ZSI 100 FTM implant. It is a malleable prosthesis that is always semi-rigid. It is unique in its design because it has a tip that mimics the glans of the penis and has a base that is a plate made of stainless steel and silicone to be fixed to the pubic bone. It is composed of a single cylinder and not attached to a pump. A recently published paper of 25 patients found that 11 (44%) had to have the prosthesis explanted because of complications in 8 and in 3 because of difficulty living with the prosthesis. This occurred with a short follow-up of only 6.3 months. on the positive side, 13/14 patients who had the prosthesis in place were able to have penetrative intercourse. (Pigot, et al. The Journal of Sexual Medicine January 2020). I would expect an even higher complication rate with longer followup.
 Impact of Phalloplasty on Penile Prosthesis
Impact of Phalloplasty on Penile Prosthesis
The type of phalloplasty can determine outcomes of prosthesis placement. Radial Forearm Flap phalloplasty tend to have thinner phalluses and it can be difficult to fit in both cylinders safely in these patients. In these patients we may choose to place only 1 of the 2 cylinders of the 3 piece penile prosthesis. The Latissimus dorsi flap phalloplasties tend to have more bulk and can more easily accommodate both cylinders of the penile prothesis as can ALT phalloplasties. Generally, I like to wait until maximal sensation returns and patients have fully healed after their phalloplasty before considering placement of a penile prosthesis.
Complications of Prosthesis Placement after Phalloplasty
The complication rates of prosthesis after phalloplasties tend to be high and range from anywhere between 30 to almost 70% in the literature. The most common complications include infection or erosion of the device that necessitates removal of the prosthesis.
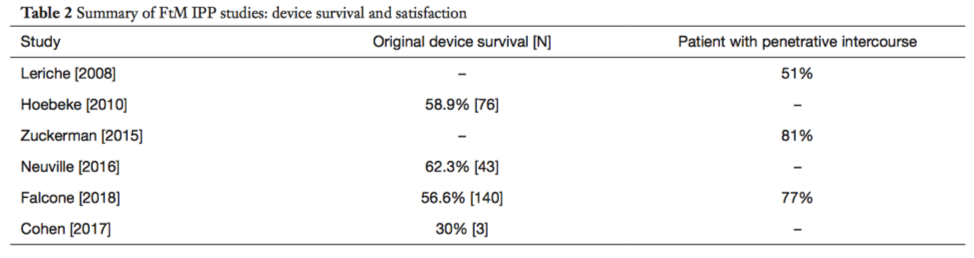
(from Kang A, et al. Translational Urology 2019; 8(3))
Conclusion
The penile prosthesis is often the final bottom surgery after many surgeries for transmen. Although the surgery has high complication rates, if the surgery goes well, it can provide the satisfaction of penetrative sexual intercourse and help realize the full function of the phallus.
For More information and to schedule a private consultation, call reconstructive surgeon Dr. Rajveer Purohit to book a in person or telemedicine consultation or appointment.
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Visit our website for more information: https://rajveerpurohitmd.com/

