GENDER AFFRMING SURGERY & RECONSTRUCTIVE UROLOGY
445 East 77th Street
New York, NY 10075
(212) 241-4812

GENDER AFFRMING SURGERY & RECONSTRUCTIVE UROLOGY
445 East 77th Street
New York, NY 10075
(212) 241-4812
Rajveer Purohit is the Director of Reconstructive Urology at the Icahn School of Medicine at Mount Sinai Hospital in New York City, and senior faculty in the Department of Urology. Dr. Purohit specializes in complex pelvic reconstructive surgery such as urethral strictures and fistula repair and gender affirmation surgery such as vaginoplasty, metoidioplasty and phalloplasty.
In 2018, Mt. Sinai appointed him co-director of its first fellowship in Reconstructive Urology that trains methods of gender affirmation surgery including vaginoplasty, metoidioplasty and phalloplasty.
Quick Links
Introduction to Genital Gender Affirmation Surgery for Transgender Women
Introduction to Genital Gender Affirmation Surgery for Transgender Men
Introduction to Transgender Care
Phalloplasty Options
See Our Main Site At RajveerPurohitMD.com
Blog Posts Are Below:
Introduction to Gender Affirmation Surgery from the Empire Lecture Series by Rajveer Purohit MD, MPH. Introductory lecture on what every urological surgeon should know about Gender Affirming Surgery in transgender patients including Penile Inversion Vaginoplasty, Metoidioplasty, and Phalloplasty.
See Dr. Purohit’s full lecture video here: Introduction to Gender Affirmation Surgery – Rajveer Purohit MD, MPH
During metoidioplasty, your surgeon creates a penis with the help of genital tissues that you already have. Prior to surgery, doctors suggest testosterone therapy to make the clitoris grow. Then, the surgeon will perform a metoidioplasty. This surgical procedure is less extensive than phalloplasty. After going through metoidioplasty, you can undergo a phalloplasty surgery. However, the process is non-reversible.
Dr. Purohit offers one of the best metoidioplasty surgeries in the United states for your gender affirmation. Patients should be 18 and older and have lived with their identified gender for at least 1 year per WPATH guidelines.
Metoidioplasty and other types of gender affiliation surgeries help gender diverse people to recognize and affirm their gender identity. The surgery of the genitals is called bottom surgery. Metoidioplasty is one of the bottom surgeries that creates a new penis by undergoing surgery on their existing genital tissues.

(Source)
When you decide to undergo metoidioplasty, the surgeon will ask you to choose from between four basic types of procedures:
Many surgeons also call the procedure simple metoidioplasty. In this method, the surgeon will release the connection of your clitoris from surrounding tissues. This method will increase the exposure and size of your penis. The simple release does not affect the vagina or create a new urethra.
In full metoidioplasty, the surgeons will release your clitoris from the surrounding tissues and link it to the urethra with the help of neophallus. They might also remove your vagina through vaginectomy and add scrotal implants.
When the surgeon performs ring metoidioplasty, they will take skin from your vaginal walls. Then they will combine the flap with the labia majora and connect with the neophallus and urethra.
In this method, the ligaments from the labia majora will spread around the labia. Then, the labia will surround the new penis. This method may provide extra girth
When opting for surgery, surgeons will give you an option to think about the changes. To get ready for the surgery, you need to adopt various changes and explore the option medically and socially. People who undergo surgery already take measures for the change, such as chest surgery and supplements for hormones. Furthermore, to go through metoidioplasty surgery, you need to be 18 years old.

(Source)
This surgery requires 2-4 hours typically. However, the duration of the surgery also depends on the surgeon you select for the metoidioplasty procedure such as vaginectomy or not. You will need general anesthesia.
In addition to the metoidioplasty a scrotoplasty is often also performed. A phalloplasty may be considered after the metoidioplasty but typically it can take up to three to six months from the first surgery to another. After the surgery, most patients stay in the hospital between 1-2 days. This depends on your surgeon and how the procedure goes.
After the surgery is complete, you will have 4 to 10 cm of a penis. However, penetrative sex with this length may be difficult. You can go through phalloplasty after the metoidioplasty. An implant after this may allow penetrative sex. With a successful metoidioplasty, you will experience a arousal and sensation in your penis.
The efficiency and accuracy of the surgery depend on the expertise of the surgeons. So you need to make sure that you are visiting a surgeon who is experienced and has the capabilities to perform your surgery.
Dr. Purohit will carefully analyze your condition and have a specialty to perform successful surgeries. Here are some qualities of our surgeon:
In short, metoidioplasty is a surgery that helps to create a penis from your genital tissues. In this procedure, you may consider a urethroplasty and vaginectomy. Having a scrotoplasty along with testicular implants is your choice. The procedure will create a 4 to 10 cm long penis. However, the sensitivity and erection will be normal.
When you undergo phalloplasty, you develop a longer penis with a similar procedure. But to experience an erection, various additional surgeries are necessary. You need to research all the methods and techniques before deciding the procedure. Although metoidioplasty is an expensive surgery, many insurance companies offer this surgery in their plan and we can help you get covered.
If you’re interested in the metoidioplasty procedure, contact top NYC reconstructive urologist Dr. Purohit for a private consultation:
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Vaginoplasty is a surgical procedure that creates a new, sensitive vagina and adjacent tissues such as clitoris and labia typically using tissue from the penis in transwomen. The vaginoplasty allows transgender and non-binary people to confirm their body image with gender and alleviates gender dysphoria.

(Source)
Usually, surgeons perform a vaginoplasty using the below-mentioned techniques:
The penile inversion procedure is a common technique in vaginoplasty. The surgeon will construct a vaginal lining using your penile skin. In this method, the surgeon will use the tip of your penis to create a clitoris and use scrotal skin to create the labia majora. The prostate will work as a G-spot, so the surgeon will leave it in place. The surgeon will also take skin from the scrotum, peritoneum or elsewhere to create the depth of the vagina when there isn’t enough skin on the penis. I generally do not consider using skin grafts to build the vulva but rather prefer to use skin that is already there to preserve sensitivity. They can recreate the skin’s sensitivity using skin from the genitals. This technique is one of the standard technique many surgeons use.
In this method, the surgeon will not use your penile skin but a short segment of your colon to create the new vagina . In this procedure, the tissue will self-lubricate. However, in the penile inversion procedure, you have to depend on artificial lubricants. We have typically been doing this surgery using a robotic surgery technique. This minimizes the scarring in the abdomen that some patient can have. The external appearance of the vagina looks very similar to the penile inversion vaginoplasty except internally the lining of the vagina looks softer.
The night before surgery, who will need to drink fluids to help you clean your bowels. In addition, Dr. Purohit asks patients to take a shower with an antibacterial soap the evening before and the morning of surgery. When you visit the clinic in the morning of surgery, Dr. Purohit and the anesthesiologist will be available for you should you have any more questions. They will provide step-by-step details about the procedure and debrief you about the process. Most people will feel anxiety while going through surgery – this is normal. When you undergo penile inversion vaginoplasty, the anesthesiologist will give you general anesthesia and you will gently fall asleep. When you wake up the surgery will be done!
The surgeon will work on your delicate nerve fiber, vasculature, and tissue, making this a complicated procedure. Testicles, if present, will be removed. Most of the penis will be removed and portions of the skin will become the lining of the vagina. The glans penis or the tip of your penis will act as the clitoris. The urethra will be reconstructed to more appropriate for female genitals.
Once they complete the procedure, the surgical team applies bandages. A catheter will be left to help drain urine and a packing will be left in the vagina. A experienced surgeon will take three to six hours to perform the surgery. You need to keep the bandages on for a few days. Typically, you are seen the week after surgery to remove the catheters and the packings.

(Source)
Your surgeon will guide you through some measures you need to take the night before the surgery or when arriving at the surgery. The anesthesiologist will give you anesthesia, they will ask you to avoid eating or drinking before the surgery. Most surgeons will take skin grafts from areas where there is potential for the hair to grow so it is important to confirm pre-operatively that hair has been adequately removed. Here are some of the tips that you should consider before going through the surgery:
When you undergo any surgery, you are at risk. Sure, in the case of vaginoplasty, there are some risk of complications but most of these can be managed safely. For infections, for example, you can take antibiotics. There are other risks of surgery as well including:
The vast majority of the time surgery results are excellent and satisfying to patients with great cosmetic outcomes and the ability to experience sexual pleasure from the new vagina and erogenous zones’ depth. Furthermore, the clitoris is made from your penile sensitive skin. Your vulva will have a labia minora as well.
Schedule an in person or tele-appointment if you are looking for an expert vaginoplasty surgeon. Dr. Purohit will help you understand the process and best vaginoplasty surgery options.
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Do you want to learn more about transgender surgery? Numerous methods and techniques are used in gender affirmation surgery. For example, for top surgery in transwomen with smaller breasts, augmentation with implants can be successful to create a more feminine appearance. For transmen whose breasts are too large, a mastectomy or removal of breast tissue, is needed.
Surgery can treat a person’s gender dysphoria, help them live with confidence, and treat their distress and depression that the dysphoria causes. Gender affirmation surgery will not only help the person transition physically but emotionally as well.

(Source)
Surgery can help those are unable to be their true selves because the gender assigned at birth does not correlate to how they feel. Surgery is the most effective way to treat gender dysphoria but some may not go through surgery and may find that hormonal treatment adequately alleviates their gender dysphoria.
Before proceeding with transgender surgery, you need to make sure you are mentally prepared. The World Professional Association of Transgender Health mandates that patients undergoing genital surgery such as vaginoplasty or phalloplasty have 2 letters from a trained mental health specialist to confirm that surgery is appropriate. The mental health counseling can also prepare you to cope with the stress and anxiety of the medical process. A professional who specializes in gender issues will guide you through the situation.
A gender mental health specialist needs to confirm that you have gender dysphoria. Gender dysphoria is a very specific condition that occurs when someone feels like they are in the wrong body, i.e., one that doesn’t align with their gender. This feeling can cause significant distress and depressed feelings.
After the therapist determines that you have gender dysphoria, they might recommend surgery and various other steps you can take to align yourself with your preferred gender. They will help increase mental satisfaction while reducing anxiety, depression, and other concerns you are facing.

(Source)
Hormones control breast size, muscle mass, body hair, and many other gender-based characteristics. These are the secondary sexual characteristics, which your surgeon will help you manage.
When transmen transition with hormones they take various androgens (masculinizing hormones) or estrogens (femininizing hormones) for the transition. Masculinizing hormones such as testosterone help deepen their voice, enlarge the clitoris, grow their body and facial hair, and strengthen their muscles.
However, when a transfemale transitions estrogens can increase the tissue in their breasts, slow down facial and body hair growth, lower testosterone levels, and much more.
Most physical changes take time to accomplish, from a month to two or even three years. For instance, when transitioning transmen have to change the body’s muscle mass, the intensity of hair growth, etc. Hormone therapy will align your appearance with your preferred gender and reduce feelings of gender dysphoria.
However, hormonal therapy has some risks and health complications. You might experience blood clots, sleep apnea, weight gain, high blood pressure, infertility, heart diseases, liver enzymes, and other health issues. Furthermore, you frequently need to visit your doctor to make sure your treatment progresses according to plan.
As part of their due diligence, surgeons make sure that you have gender dysphoria through letters from a mental health professional and have been living a life as your true gender for at least 1 year. After getting the necessary health and mental clearance, they will perform surgery. If your preferred gender is different from the one your parents assigned at birth, fully aligning your body with your preferred gender may require various surgical procedures. Your surgeon will give you the option of choosing between different surgeries and help you decide which ones you would prefer. They will explain the procedures and their effect on your quality of life after the surgery. Ideally surgeries have better results in terms of function and cosmetic appearance.
Different surgeries have varying risks of complications and success rates. You must choose after thoroughly studying the methods.
When you undergo gender affirmation surgery, your health and post-surgery quality of life depends on the type of surgery you chose and the surgeon you pick. Most patients are satisfied with the result after going through the procedure but there are risks of complications. Hence, you must carefully choose your surgeon. By choosing a professional surgeon, you increase the success rate. Lastly, you need to visit your surgeon for post-operation guidelines and keep tabs on your progress.
If you feel like you are experiencing gender dysphoria, contact Dr. Rajveer Purohit for complete details about the procedure and benefits of gender affirmation surgery. He is a highly qualified and experienced surgeon who can help you with the surgery and any change that will help you live a life that reflects your gender.
There are many different testicular implants produced throughout the world but generally they come in two varieties: a solid ovoid block of silicone or a silicone shell filled with saline. In the United States, however, there is only one FDA approved prosthesis available, the Torosa prosthesis made by Coloplast. This is testicular prosthesis that we use during a metoidioplasty.
The Torosa testicular prosthesis comes in a variety sizes and is filled with saline. The amount of saline filled during surgery can change the feel of the prosthesis and give more or less density to the prosthesis.
Typically for transmen undergoing metoidioplasty, the testicular prosthesis will be placed at the same time rather than as a separate surgical procedure.

While some patients want as large a prosthesis as possible, there is a balance between the size of the new phallus and the prosthesis. If the testicular prosthesis is too big, the phallus will appear buried and not protrude out through the body.
I typically make a slightly curved incision on each side above where the prosthesis will go – an alternative is to make an incision medially where the urethra is being reconstructed and place the prosthesis through this so there is fewer incisions. With the second way there is less scar but, in my opinion, a somewhat higher risk of erosion and infection of the prosthesis after the metoidioplasty.
After surgery a capsule forms around the prosthesis to keep it in place. This process takes a few weeks to occur – during this time we ask metoidioplasty patients to confirm that the prosthesis is kept down in the scrotal sac periodically. Also, metoidioplasty patients are asked to walk in with their legs slightly spread apart because the thighs can push the prosthesis up and migrate higher and into the inguinal area. If the capsule forms around the testes when they are higher in the scrotum than it will become permanently more mobile and periodically migrate higher into the inguinal area. If this does happen then you might need a minor surgery to correct this and remove the excess capsule and bring the prosthesis down into the proper position.
Other potential complications include infection or erosion of the testicular prosthesis which mandates removal of the testicular prosthesis and potentially replacing during a later surgery. Sometimes, patients can have minor pain or bleeding around the site of prosthesis.
Overall, though, most transmen are very satisfied with appearance and feel of the testicular prosthesis after metoidioplasty.
To schedule a confidential appointment, contact Dr. Rajveer Purohit today. Dr. Purohit is a highly trained New York City reconstructive urologist specializing in transgender surgery.
Rajveer Purohit, MD, MPH
(212) 241-4812
* Telemedicine and in person consultations available
Placement of a penile prosthesis is often the final surgery after a long journey for many transmen – it is the culmination and hopefully last genital surgery. It is also a surgery with a high risk of complications and can potentially compromise the outcome of prior surgeries to create the neo-phallus.
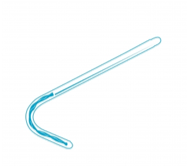
There are 2 type of masculinizing genital surgeries: the metoidioplasty and some form of a phalloplasty. There is no FDA approved penile implant for a metoidioplasty. There is, however, a new device made by ZSI, which is available in Europe and designed specifically for a metoidioplasty. Essentially the device is made up of 2 silicone rods, each about 4mm in width, with a silver cable in the middle for stiffness. The solid cable is cut intra-operatively based on the length of the neo-phallus. There is not very much data available on this prosthesis and only time will tell if it will work. However, it is currently not available in the United States.
There are 2 kinds of penile prosthesis for phalloplasties: malleable prosthesis and an inflatable prosthesis. The malleable prosthesis is a semi-rigid prosthesis that is always partially erect. Men can bend it down when not having sex and bend it upwards when they want to have sex. It is easy to place surgically and has less component parts so it is less likely to get infected. The problem is that it is never fully soft and never completely hard. Also, in my opinion, different from cis-men it has a higher risk of infection that inflatable prosthesis.
The inflatable prosthesis allows deflation of the prosthesis and inflation when patients want a rigid phallus. As such, it is more “natural” and patients can have a flaccid phallus when they are not stimulated. The prosthesis come in two varieties – one made up of two components (2 piece inflatable prosthesis) and one made up of three components (3 piece inflatable prosthesis). In the United States, there are two companies that make an FDA approved prosthesis: Coloplast and AMS. There are some differences in the types of prosthesis that both of these companies make including impregnation of the prosthesis with antibiotics to reduce the risk of infection, the ease of use of the pump and varying levels of girth expansion.
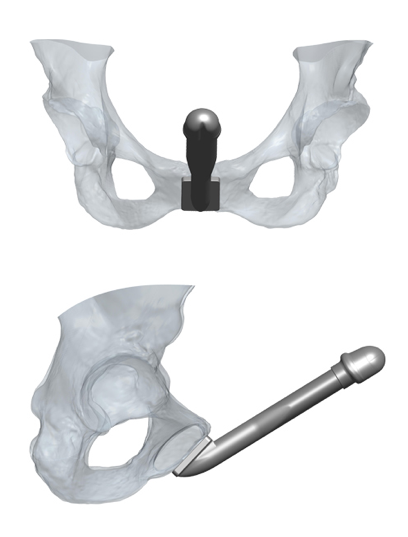
Placement of a penile prosthesis in transmen is different then placement in cis-men for a few reasons. First, cis-men’s penis’s contain 2 internal cylinders called the corpora cavernosa. These are the bodies that would normally create erections as they fill up with blood. These cylinders are made up of a tough tissue called the tunica which contains the implants. The corpora prevent migration or erosion of the cylinders into the skin and fix the cylinders in placed so that during sex they don’t move around. When placing a prosthesis in transmen we try to recreate this function by suturing the prosthesis down to the pubic bone to keep it in place and prevent migration. But it is not perfect.
The 3-piece inflatable prosthesis is the most common type of prosthesis used. It is made up of two inflatable cylinders placed in the penis, a pump placed in the scrotum and a reservoir that contains fluid. When the pump is pressed fluid is transferred from the reservoir to the cylinders. When deactivated, the fluid is transferred back to the reservoir causing the prosthesis to deflate and the erection to go away.
There has been an implant designed specifically for phalloplasty: the ZSI 100 FTM implant. It is a malleable prosthesis that is always semi-rigid. It is unique in its design because it has a tip that mimics the glans of the penis and has a base that is a plate made of stainless steel and silicone to be fixed to the pubic bone. It is composed of a single cylinder and not attached to a pump. A recently published paper of 25 patients found that 11 (44%) had to have the prosthesis explanted because of complications in 8 and in 3 because of difficulty living with the prosthesis. This occurred with a short follow-up of only 6.3 months. on the positive side, 13/14 patients who had the prosthesis in place were able to have penetrative intercourse. (Pigot, et al. The Journal of Sexual Medicine January 2020). I would expect an even higher complication rate with longer followup.
 Impact of Phalloplasty on Penile Prosthesis
Impact of Phalloplasty on Penile ProsthesisThe type of phalloplasty can determine outcomes of prosthesis placement. Radial Forearm Flap phalloplasty tend to have thinner phalluses and it can be difficult to fit in both cylinders safely in these patients. In these patients we may choose to place only 1 of the 2 cylinders of the 3 piece penile prosthesis. The Latissimus dorsi flap phalloplasties tend to have more bulk and can more easily accommodate both cylinders of the penile prothesis as can ALT phalloplasties. Generally, I like to wait until maximal sensation returns and patients have fully healed after their phalloplasty before considering placement of a penile prosthesis.
The complication rates of prosthesis after phalloplasties tend to be high and range from anywhere between 30 to almost 70% in the literature. The most common complications include infection or erosion of the device that necessitates removal of the prosthesis.
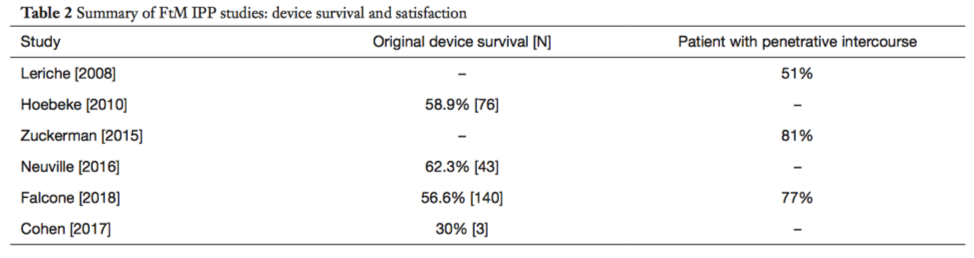
(from Kang A, et al. Translational Urology 2019; 8(3))
The penile prosthesis is often the final bottom surgery after many surgeries for transmen. Although the surgery has high complication rates, if the surgery goes well, it can provide the satisfaction of penetrative sexual intercourse and help realize the full function of the phallus.
For More information and to schedule a private consultation, call reconstructive surgeon Dr. Rajveer Purohit to book a in person or telemedicine consultation or appointment.
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Visit our website for more information: https://rajveerpurohitmd.com/
In early March, Dr. Purohit was honored to be invited as a renowned international expert to teach a Masterclass on Gender Affirmation Surgery in India to over 120 Plastic Surgeons. He presented 4 lectures focusing on his techniques to optimize cosmetic and functional outcomes.
Gender Affirmation Surgery Topics included:
The talks were very well received and he was asked to light the “Diya” or light of knowledge at the end of the conference.
Dr Rajveer Purohit Clears All Doubts On Coronavirus, Lauds India’s Lockdown Measure
https://www.facebook.com/IndiaToday/videos/was-newyork-not-prepared-for-pandemic-/504016633600850/
https://www.facebook.com/ndtv/videos/covid-19-on-the-availability-of-ventilators/512192282779930/
Often with penile inversion vaginoplasty, skin from the scrotal or pelvic area is used to create the new vagina. Some of this area, however, contains hair which can continue to grow even after the skin is used to create the new vagina. In addition to being unsightly, the vaginal hair can create an odor, mucous, even stones inside the vagina. Once it has formed it is difficulty to permanently remove hair once it grows inside the vagina. For this reason, preoperative permanent hair removal is critical for having a good postoperative outcome.
For penile inversion vaginoplasty we use the following template for where the hair should be removed:
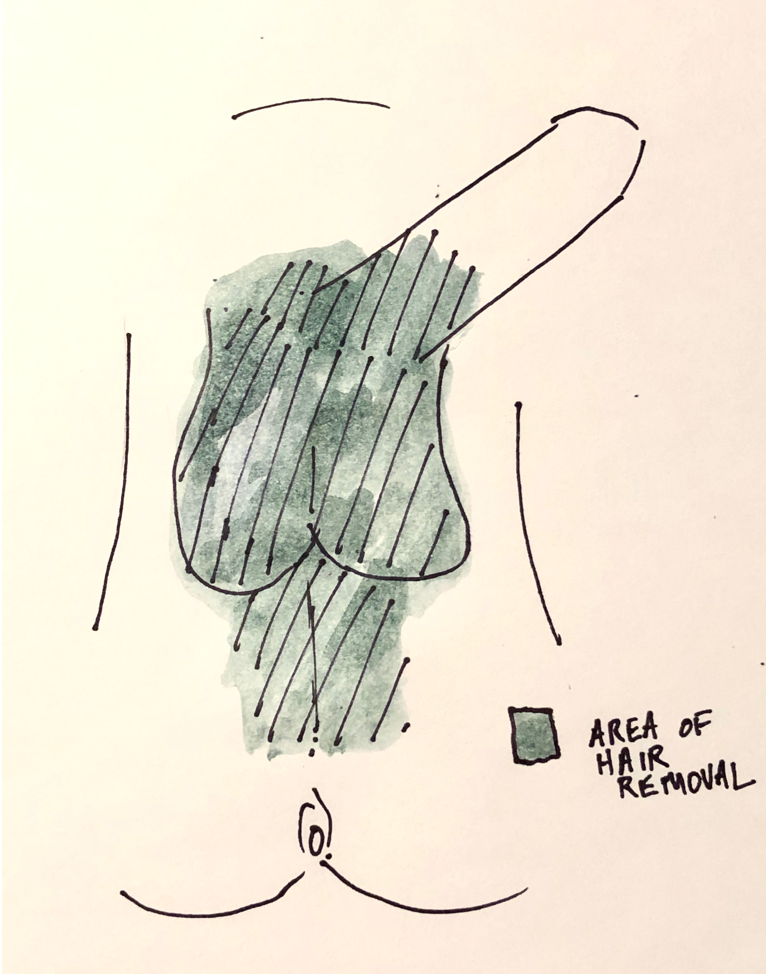 Should I Remove All of the Hair Before my Vaginoplasty? What is the Best Method?
Should I Remove All of the Hair Before my Vaginoplasty? What is the Best Method?Generally, I advise patients to leave some hair above the phallus as this will leaves aesthetically appropriate hair in the mons region above the vagina after penile inversion vaginoplasty. If you don’t want that pubic hair you can always have it easily removed after surgery.
Shaving, tweezing or waxing the hair helps to remove hair in the short run but the hair tends to grow back. There are two methods of permanent hair removal that are commonly used: electrolysis and laser.
Electrolysis uses electrical energy to destroy the root of the hair and, unlike Laser treatments, it has the same effect on patients regardless of skin or hair color. But, with electrolysis only small patches of hair can be removed at once and patients typically require multiple visits for complete hair removal.
Laser hair removal uses a laser to destroy the roots of the hair. Because it targets darker pigment, it is generally best for patients with light skin and coarse, dark hair – the laser can sometimes burn darker colored skin and leave the skin with patchy lighter colored areas. The advantage of laser hair removal is that it permits large areas of hair removal at once and can be quicker to remove large areas of hair prior to surgery. If hair does come back, it tends to come back a little lighter than before.
We are fortunate to have a laser available at Mount Sinai for our patients undergoing gender affirmation surgery. Health insurance generally does not cover hair removal, we have had some success getting coverage for laser hair removal when it is done at Mount Sinai. If your insurance does not cover hair removal, electrolysis is generally cheaper than laser hair removal – although costs can vary greatly.
Hair removal can take time to schedule and I always tell my patients to start the process as soon as possible after their initial visit with me. It is sometimes the step that delays getting your vaginoplasty completed. If you do not live close to New York City hair removal can be done locally to speed up the process.
For more information, call today:
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Vaginal dilations are a very important part of your recovery process after vaginoplasty. Dilations keep the vagina open preventing vaginal stenosis – a process where the vaginal walls scars down and contract. The new vagina has a tendency to close because the body’s reaction to any procedure is to scar and try to heal itself – although in this situation this “healing” process is counterproductive.
After your vaginoplasty you will be sent home with a new set of vaginal dilators. Bring these dilators with you on your first visit to the office.
When you are discharged home you will have a catheter in place to drain the bladder and a packing left in the vagina. This packing is very important as it allows the vagina skin to heal and “stick” to the underlying tissue. During this time, as you recover, it is important to avoid any vigorous activity in part because you don’t want to have incisions disrupted but also because it allows time for the vaginal grafts to “take” which in the long term increase the chances of a good outcome.
 Soul Source Dilators
Soul Source DilatorsThe dilators you will be sent home with are usually from a company called Soul Source and come in four different sizes and colors (https://www.soulsource.com/collections/grs-vaginal-dilators). The dilators are gently angled at the tip to conform with with angle of the vagina. In addition, their are dots alongside the length of the dilators which correspond to the depth. If you are able to get the dilator to the final dot on the dilator then that is 6 inches of vaginal depth (a pretty good result!).
About one week after surgery when you come into the office he vaginal packing will be removed. This can be a little uncomfortable and the packing itself can have an odor to it. Once removed, I’ll show how to use the dilators by starting on the purple size (the thinnest dilator).
After you get home you should dilate once. Always use lubrication when you dilation. Often patients will start with metronidazole gel which can be used as a lubricant as well. For the first 2 weeks after surgery you should dilated twice a day for about 20-30 minutes each time. After 2 weeks you can increase the frequency of dilation to 3 times a day. After a month you can start to go up on the size oft eh dilatory to blue then green and finally orange. Consider increasing the size of the dilator if the dilator goes in easily to the final dot and you don’t have any discomfort placing it.
If the dilations are getting more difficult or the vagina is feeling tighter when you dilate you should dilate more frequently every day until it is easier to get the dilator in. You can also leave the dilator in for longer periods of time if it is difficult to dilate.
Make sure the dilator is clean before dilation and after dilation you can just wash out the dilator with a mild soup and water. It should be kept clean but does not have to be sterile.
You should also douche with a minimal amount of gentle soap and mostly water to keep the vagina clean starting about 2 weeks after surgery. Women typically will do this in the shower or on the toilet. Periodic douching washes out remnants of the lubrication and can hep decrease bacterial overgrowth.
Vaginal dilations are important to minimize one of the more common risks after vaginoplasty – vaginal stenosis or closure of the vaginal canal. But do different techniques of penile inversion vaginoplasty have different risks of vaginal stenosis? Unfortunately, like so many things in the field, there isn’t great comparative data on this topic. At a very basic level there are 2 types of tissues that we typically use to create the vaginal lining: tissue flaps or tissue grafts. The difference between the two is that flaps are still connected to their own blood supply while grafts are not- grafts survive initially by sucking up oxygen from surrounding tissue until new blood vessels develop over the course of a few days. Because of this blood supply difference, grafts have a higher chance for contraction and vaginal stenosis. The penile skin in the penile inversion vaginoplasty is a flap and scrotal or peritoneal skin are grafts.
So how do you minimize the risk of vaginal stenosis? Use as much of a flap as you can to create the vaginal lining. So this mean using as much penile skin as possible. Sometimes, patients have enough tissue to create a deep 6 inch vagina but in many cases there isn’t enough tissue to do this. In this case, before surgery you should decide whats important for you – If you want to absolutely minimize risk of stenosis and penetrative vaginal sex or vaginal depth is not important to you then you might stick with the penile flap and not add additional depth with a graft. if depth is important and there is not much phallic skin then you would almost certainly want additional depth with a graft and accept the risk of stenosis and post-op be very diligent about dilations.
Although there are disadvantages to using colon for a vaginoplasty, one of the advantages is that the segment of colon has its own blood supply so that the risk of stenosis is very low.
 Dr. Rajveer Purohit is the Director of Voiding Dysfunction and Reconstructive Urology and Senior Faculty at the Icahn School of Medicine at The Mount Sinai Hospital. He is experienced performing over 700 complex reconstructive surgical procedures including urethroplasty for urethral strictures with grafts and flaps, gender affirming surgery including vaginoplasty, metoidioplasty and phalloplasty, treatment of pelvic mesh and radiation complications.
Dr. Rajveer Purohit is the Director of Voiding Dysfunction and Reconstructive Urology and Senior Faculty at the Icahn School of Medicine at The Mount Sinai Hospital. He is experienced performing over 700 complex reconstructive surgical procedures including urethroplasty for urethral strictures with grafts and flaps, gender affirming surgery including vaginoplasty, metoidioplasty and phalloplasty, treatment of pelvic mesh and radiation complications.
Dr. Purohit graduated Magna Cum Laude from Williams College and earned his medical degree (MD) and Masters in Public Health (MPH) from Columbia University before completing his surgical internship and urology residency at the University of California in San Francisco. While there he trained with one of the pioneers of male urethral reconstruction and then completed a fellowship with Dr. Jerry Blaivas in pelvic reconstruction and voiding dysfunction.
![]() He has been chosen by his colleagues for inclusion in Castle Connolly’s Best Doctors and listed yearly in New York Magazine’s Best Doctors in New York City. He has been awarded the Pfizer Scholars in Urology, AUA/Praecis Gerald P. Murphy Scholar, Society of Medicine and Reproductive Urology Travel Scholar award, a California Urology Foundation Grant and an Arnold P. Gold Fellowship and multiple Patient Choice and Compassionate Doctor awards.
He has been chosen by his colleagues for inclusion in Castle Connolly’s Best Doctors and listed yearly in New York Magazine’s Best Doctors in New York City. He has been awarded the Pfizer Scholars in Urology, AUA/Praecis Gerald P. Murphy Scholar, Society of Medicine and Reproductive Urology Travel Scholar award, a California Urology Foundation Grant and an Arnold P. Gold Fellowship and multiple Patient Choice and Compassionate Doctor awards.

Dr. Purohit is a member of the following associations & organizations:
Dr. Purohit continues to actively research and publish on a variety of topics in pelvic reconstruction and urology.
Follow Dr. Purohit on Twitter: @DrUroRecon
Wikipedia: Dr. Rajveer Purohit
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812