GENDER AFFRMING SURGERY & RECONSTRUCTIVE UROLOGY
445 East 77th Street
New York, NY 10075
(212) 241-4812

GENDER AFFRMING SURGERY & RECONSTRUCTIVE UROLOGY
445 East 77th Street
New York, NY 10075
(212) 241-4812
Rajveer Purohit is the Director of Reconstructive Urology at the Icahn School of Medicine at Mount Sinai Hospital in New York City, and senior faculty in the Department of Urology. Dr. Purohit specializes in complex pelvic reconstructive surgery such as urethral strictures and fistula repair and gender affirmation surgery such as vaginoplasty, metoidioplasty and phalloplasty.
In 2018, Mt. Sinai appointed him co-director of its first fellowship in Reconstructive Urology that trains methods of gender affirmation surgery including vaginoplasty, metoidioplasty and phalloplasty.
Quick Links
Introduction to Genital Gender Affirmation Surgery for Transgender Women
Introduction to Genital Gender Affirmation Surgery for Transgender Men
Introduction to Transgender Care
Phalloplasty Options
Resumption of Surgery and Office Visits
I want to thank my many patients who reached out to me over the last few months – it was profoundly moving and reminded me of how strong a bond I have been lucky to form with so many wonderful people many of whom just happen to also be my patients.
I am pleased to announce that we have resumed our full surgery schedule as of June 8 and our full schedule of regular office visits will resume as of June 22. We have made substantial changes to our practice including steps to minimize the risk of Covid exposure to patients and also will continue to offer telehealth visits in the future.
Rajveer Purohit MD, MPH
See Our Main Site At RajveerPurohitMD.com
Blog Posts Are Below:
Vaginoplasty is a surgical procedure that creates a new, sensitive vagina and adjacent tissues such as clitoris and labia typically using tissue from the penis in transwomen. The vaginoplasty allows transgender and non-binary people to confirm their body image with gender and alleviates gender dysphoria.

(Source)
Usually, surgeons perform a vaginoplasty using the below-mentioned techniques:
The penile inversion procedure is a common technique in vaginoplasty. The surgeon will construct a vaginal lining using your penile skin. In this method, the surgeon will use the tip of your penis to create a clitoris and use scrotal skin to create the labia majora. The prostate will work as a G-spot, so the surgeon will leave it in place. The surgeon will also take skin from the scrotum, peritoneum or elsewhere to create the depth of the vagina when there isn’t enough skin on the penis. I generally do not consider using skin grafts to build the vulva but rather prefer to use skin that is already there to preserve sensitivity. They can recreate the skin’s sensitivity using skin from the genitals. This technique is one of the standard technique many surgeons use.
In this method, the surgeon will not use your penile skin but a short segment of your colon to create the new vagina . In this procedure, the tissue will self-lubricate. However, in the penile inversion procedure, you have to depend on artificial lubricants. We have typically been doing this surgery using a robotic surgery technique. This minimizes the scarring in the abdomen that some patient can have. The external appearance of the vagina looks very similar to the penile inversion vaginoplasty except internally the lining of the vagina looks softer.
The night before surgery, who will need to drink fluids to help you clean your bowels. In addition, Dr. Purohit asks patients to take a shower with an antibacterial soap the evening before and the morning of surgery. When you visit the clinic in the morning of surgery, Dr. Purohit and the anesthesiologist will be available for you should you have any more questions. They will provide step-by-step details about the procedure and debrief you about the process. Most people will feel anxiety while going through surgery – this is normal. When you undergo penile inversion vaginoplasty, the anesthesiologist will give you general anesthesia and you will gently fall asleep. When you wake up the surgery will be done!
The surgeon will work on your delicate nerve fiber, vasculature, and tissue, making this a complicated procedure. Testicles, if present, will be removed. Most of the penis will be removed and portions of the skin will become the lining of the vagina. The glans penis or the tip of your penis will act as the clitoris. The urethra will be reconstructed to more appropriate for female genitals.
Once they complete the procedure, the surgical team applies bandages. A catheter will be left to help drain urine and a packing will be left in the vagina. A experienced surgeon will take three to six hours to perform the surgery. You need to keep the bandages on for a few days. Typically, you are seen the week after surgery to remove the catheters and the packings.

(Source)
Your surgeon will guide you through some measures you need to take the night before the surgery or when arriving at the surgery. The anesthesiologist will give you anesthesia, they will ask you to avoid eating or drinking before the surgery. Most surgeons will take skin grafts from areas where there is potential for the hair to grow so it is important to confirm pre-operatively that hair has been adequately removed. Here are some of the tips that you should consider before going through the surgery:
When you undergo any surgery, you are at risk. Sure, in the case of vaginoplasty, there are some risk of complications but most of these can be managed safely. For infections, for example, you can take antibiotics. There are other risks of surgery as well including:
The vast majority of the time surgery results are excellent and satisfying to patients with great cosmetic outcomes and the ability to experience sexual pleasure from the new vagina and erogenous zones’ depth. Furthermore, the clitoris is made from your penile sensitive skin. Your vulva will have a labia minora as well.
Schedule an in person or tele-appointment if you are looking for an expert vaginoplasty surgeon. Dr. Purohit will help you understand the process and best vaginoplasty surgery options.
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Often with penile inversion vaginoplasty, skin from the scrotal or pelvic area is used to create the new vagina. Some of this area, however, contains hair which can continue to grow even after the skin is used to create the new vagina. In addition to being unsightly, the vaginal hair can create an odor, mucous, even stones inside the vagina. Once it has formed it is difficulty to permanently remove hair once it grows inside the vagina. For this reason, preoperative permanent hair removal is critical for having a good postoperative outcome.
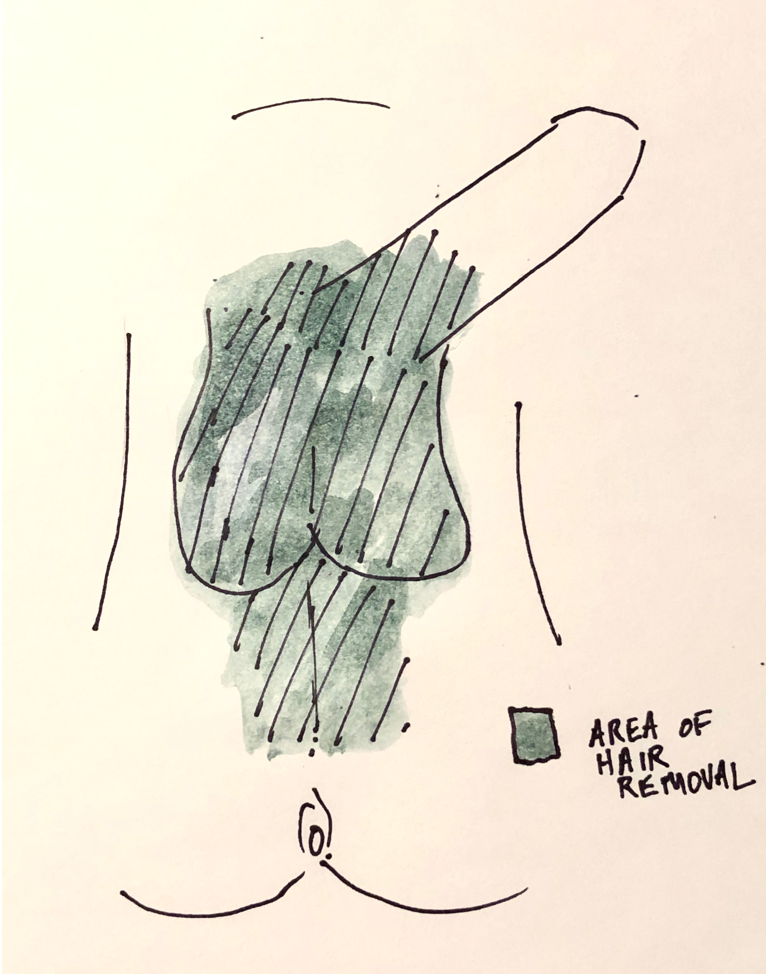
For penile inversion vaginoplasty we use the following template for where the hair should be removed:
 Should I Remove All of the Hair Before my Vaginoplasty? What is the Best Method?
Should I Remove All of the Hair Before my Vaginoplasty? What is the Best Method?Generally, I advise patients to leave some hair above the phallus as this will leaves aesthetically appropriate hair in the mons region above the vagina after penile inversion vaginoplasty. If you don’t want that pubic hair you can always have it easily removed after surgery.
Shaving, tweezing or waxing the hair helps to remove hair in the short run but the hair tends to grow back. There are two methods of permanent hair removal that are commonly used: electrolysis and laser.
Electrolysis uses electrical energy to destroy the root of the hair and, unlike Laser treatments, it has the same effect on patients regardless of skin or hair color. But, with electrolysis only small patches of hair can be removed at once and patients typically require multiple visits for complete hair removal.
Laser hair removal uses a laser to destroy the roots of the hair. Because it targets darker pigment, it is generally best for patients with light skin and coarse, dark hair – the laser can sometimes burn darker colored skin and leave the skin with patchy lighter colored areas. The advantage of laser hair removal is that it permits large areas of hair removal at once and can be quicker to remove large areas of hair prior to surgery. If hair does come back, it tends to come back a little lighter than before.
We are fortunate to have a laser available at Mount Sinai for our patients undergoing gender affirmation surgery. Health insurance generally does not cover hair removal, we have had some success getting coverage for laser hair removal when it is done at Mount Sinai. If your insurance does not cover hair removal, electrolysis is generally cheaper than laser hair removal – although costs can vary greatly.
Hair removal can take time to schedule and I always tell my patients to start the process as soon as possible after their initial visit with me. It is sometimes the step that delays getting your vaginoplasty completed. If you do not live close to New York City hair removal can be done locally to speed up the process.
For more information, call today:
Rajveer Purohit, MD, MPH
445 East 77th Street
New York, NY 10075
(212) 241-4812
Vaginal dilations are a very important part of your recovery process after vaginoplasty. Dilations keep the vagina open preventing vaginal stenosis – a process where the vaginal walls scars down and contract. The new vagina has a tendency to close because the body’s reaction to any procedure is to scar and try to heal itself – although in this situation this “healing” process is counterproductive.
After your vaginoplasty you will be sent home with a new set of vaginal dilators. Bring these dilators with you on your first visit to the office.
When you are discharged home you will have a catheter in place to drain the bladder and a packing left in the vagina. This packing is very important as it allows the vagina skin to heal and “stick” to the underlying tissue. During this time, as you recover, it is important to avoid any vigorous activity in part because you don’t want to have incisions disrupted but also because it allows time for the vaginal grafts to “take” which in the long term increase the chances of a good outcome.
 Soul Source Dilators
Soul Source DilatorsThe dilators you will be sent home with are usually from a company called Soul Source and come in four different sizes and colors (https://www.soulsource.com/collections/grs-vaginal-dilators). The dilators are gently angled at the tip to conform with with angle of the vagina. In addition, their are dots alongside the length of the dilators which correspond to the depth. If you are able to get the dilator to the final dot on the dilator then that is 6 inches of vaginal depth (a pretty good result!).
About one week after surgery when you come into the office he vaginal packing will be removed. This can be a little uncomfortable and the packing itself can have an odor to it. Once removed, I’ll show how to use the dilators by starting on the purple size (the thinnest dilator).
After you get home you should dilate once. Always use lubrication when you dilation. Often patients will start with metronidazole gel which can be used as a lubricant as well. For the first 2 weeks after surgery you should dilated twice a day for about 20-30 minutes each time. After 2 weeks you can increase the frequency of dilation to 3 times a day. After a month you can start to go up on the size oft eh dilatory to blue then green and finally orange. Consider increasing the size of the dilator if the dilator goes in easily to the final dot and you don’t have any discomfort placing it.
If the dilations are getting more difficult or the vagina is feeling tighter when you dilate you should dilate more frequently every day until it is easier to get the dilator in. You can also leave the dilator in for longer periods of time if it is difficult to dilate.
Make sure the dilator is clean before dilation and after dilation you can just wash out the dilator with a mild soup and water. It should be kept clean but does not have to be sterile.
You should also douche with a minimal amount of gentle soap and mostly water to keep the vagina clean starting about 2 weeks after surgery. Women typically will do this in the shower or on the toilet. Periodic douching washes out remnants of the lubrication and can hep decrease bacterial overgrowth.
Vaginal dilations are important to minimize one of the more common risks after vaginoplasty – vaginal stenosis or closure of the vaginal canal. But do different techniques of penile inversion vaginoplasty have different risks of vaginal stenosis? Unfortunately, like so many things in the field, there isn’t great comparative data on this topic. At a very basic level there are 2 types of tissues that we typically use to create the vaginal lining: tissue flaps or tissue grafts. The difference between the two is that flaps are still connected to their own blood supply while grafts are not- grafts survive initially by sucking up oxygen from surrounding tissue until new blood vessels develop over the course of a few days. Because of this blood supply difference, grafts have a higher chance for contraction and vaginal stenosis. The penile skin in the penile inversion vaginoplasty is a flap and scrotal or peritoneal skin are grafts.
So how do you minimize the risk of vaginal stenosis? Use as much of a flap as you can to create the vaginal lining. So this mean using as much penile skin as possible. Sometimes, patients have enough tissue to create a deep 6 inch vagina but in many cases there isn’t enough tissue to do this. In this case, before surgery you should decide whats important for you – If you want to absolutely minimize risk of stenosis and penetrative vaginal sex or vaginal depth is not important to you then you might stick with the penile flap and not add additional depth with a graft. if depth is important and there is not much phallic skin then you would almost certainly want additional depth with a graft and accept the risk of stenosis and post-op be very diligent about dilations.
Although there are disadvantages to using colon for a vaginoplasty, one of the advantages is that the segment of colon has its own blood supply so that the risk of stenosis is very low.